Adhesive capsulitis, or frozen shoulder, is a common but poorly understood condition that can affect the shoulder in a variety of patients.Its name suggests the fact that the shoulder loses range of motion, and deep pain is a common component of this troublesome malady.
Cause
Very frequently, the condition develops because of trauma to the shoulder, which can include prior surgical intervention; however, many patients develop this condition spontaneously for unknown reasons.
It is commonly seen in older women as well as patients with certain metabolic conditions including diabetes, thyroid hormone imbalances, and even Parkinson’s disease. While the causes are not well understood, the pathology is typically characterized by thickening of the joint capsule.
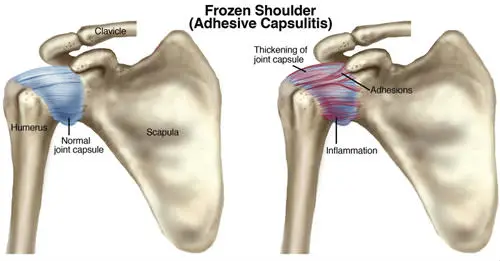
This thickening leads to a loss in tissue mobility and consequently inhibits the shoulder range of motion.
Three stages Adhesive capsulitis generally presents in a series of three stages. The first is a painful stage where deep persistent pain develops and often does not allow the patient to sleep well.
The range of motion is not affected until the second stage, known as the freezing stage. In this stage, the shoulder loses a significant amount of its motion capability.
In the third stage, known as the thawing stage, the patient begins to incrementally regain much of the range of motion, but during this stage pain can reappear.
Conservative treatment
While many patients go through all stages, and eventually regain a near normal range of motion, it is important to monitor the progress and be ready to intervene because some of this motion loss can be permanent.
This is particularly true in patients who have had a fracture or a surgical procedure so that capsulitis does not limit the return of function. Frequently, this cascade of events worsens and then resolves within a one to two year period.
During that time, anti-inflammatories or a corticosteroid injection in the shoulder joint can offer some relief. Corticosteroid injections can be detrimental to normal tissues in the long run, though, and should be used sparingly.
Particular exercises instituted by a physical or occupational therapist are crucial in order to maintain range of motion and stimulate recovery.

Surgical Options
When the range of motion does not respond to conservative measures and pain magnifies, surgical treatment may be indicated. Traditional treatment involves manipulating the shoulder while under an anesthetic, which can lead to an improvement in motion that might only be temporary.
The reason is that manipulation itself can cause tearing of the soft tissue structures that often heal by forming additional scar tissue. Therefore, it is best to perform manipulation in conjunction with an arthroscopic procedure where the tissues are released during the surgery (arthroscopic capsulectomy), which limits the scarring.
This is a minimally invasive procedure where a tiny camera is inserted into the joint so that the joint capsule can be visualized from the inside, allowing the release of the tissue using either mechanical instruments or even radiofrequency probes in a traumatic fashion.
After Surgery
Once motion is restored, it is important to maintain it. Maintaining motion may include the use of a continuous passive motion (CPM) machine, which the patient will often use at home. Therapy begins within a few days after surgery.