Anti-inflammatories, splinting, or even corticosteroid injections simply diminish symptoms but do not provide a long-term solution.
What is osteoarthritis ?
Most typically basal joint arthritis, is the second most common location for arthritis in the hand but the most functionally disabling. The function of thumb opposition and subsequent pinch are crucial for such daily activities as turning a key, opening a jar, or picking a small object off the table, No wonder pain and weakness from the base of the thumb is so functionally disabling!
Conservative treatment for Basal Joint Arthritis:
The initial treatment of symptomatic basal joint arthritis is most often for pain relief. Anti-inflammatories, splinting, or even corticosteroid injections simply diminish symptoms but do not provide a long-term solution. They do not alter the often inevitable course of progressive pain and even deformity.
Therapy can play a role in conservative treatment, but in severe cases it can actually aggravate symptoms.
A wide variety of splints are available that allow the joint to rest and may minimize the pain, but the very fact that motion of this joint is important for hand function underscores the need for something other than splinting.
Nonsterodial anti-inflammatories (ibuprofen/ Naproxen/Cox-2 inhibitors) have only a temporary effect and are used simply for marginal symptomatic relief.
The gastric complications of using these drugs should not be overlooked and patients should not use them long-term when seeking relief from simply one joint in the hand.

Injections for thumb pain?
Corticosteroid injections have a more prolonged effect but can have long-term deleterious effects on the joint cartilage or capsule.
Persistent pain demands that something more definitive be instituted for treatment;. and for this reason, surgery has generally been the most effective treatment in symptomatic cases.
Surgical Option: LRTI
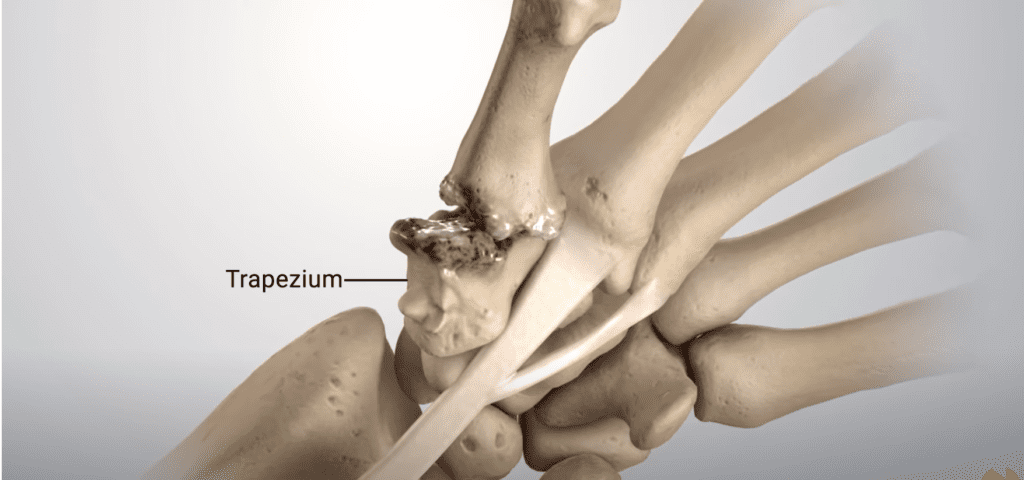
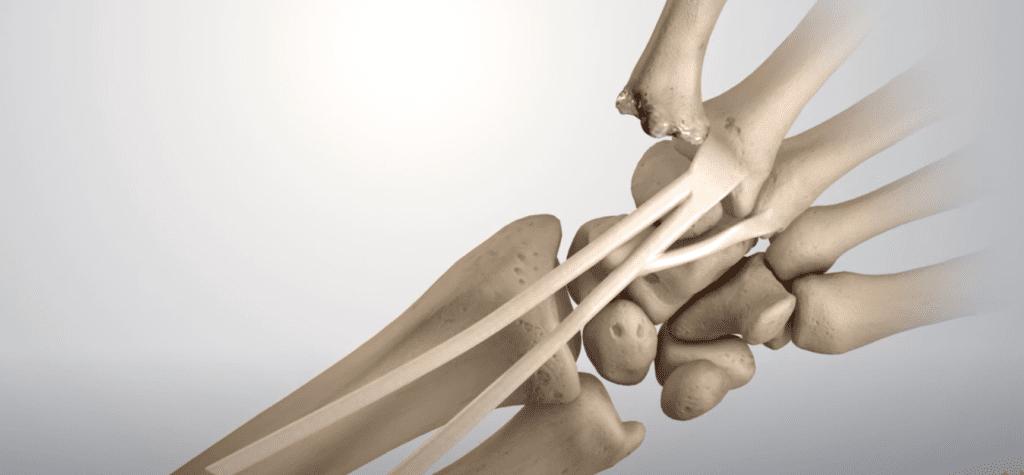
The problem is that until recently, there have
been few surgical options, and those were often quite painful and required a prolonged recovery. One of the earliest surgical treatments was complete excision of the trapezium, a small bone at the base of the thumb within the wrist.
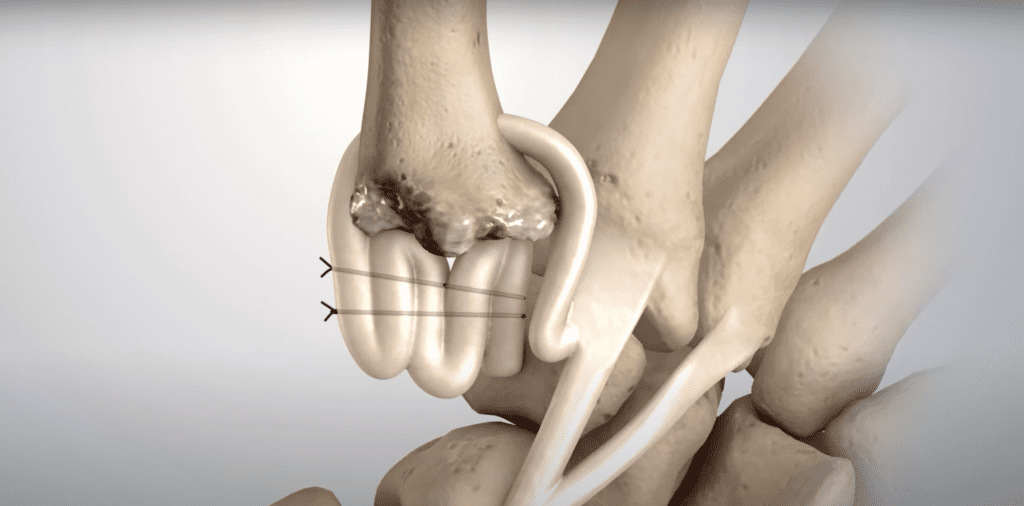
This simple operation was first described over 50 years ago. A more complex version of this procedure is termed the LRTI (ligament reconstruction tendon interposition) and has become the most commonly used surgical procedure for treatment of painful basal joint arthritis.
This relatively complex operation combines several previously described procedures including the complete removal of the trapezium bone and the stabilization of the metacarpal base using a strip of a wrist tendon.
While reports in the hand surgery literature are generally favorable in terms of the outcome, several problems remain with this operation. One of them is that the recovery. process is relatively long and can be painful.
However, the main problem lies in the fact that there are few salvage options if painful symptoms persist because the trapezium has been completely removed.
Once this bone, the pillar base of the thumb, is removed, there are few remedies available to reconstruct the thumb should the need arise.
Similar problems occur after fusion, which eliminates motion because the adjacent joints, which are frequently arthritic as well, can become symptomatic. Reversing a fusion is a formidable task and joint replacement maybe the only option.
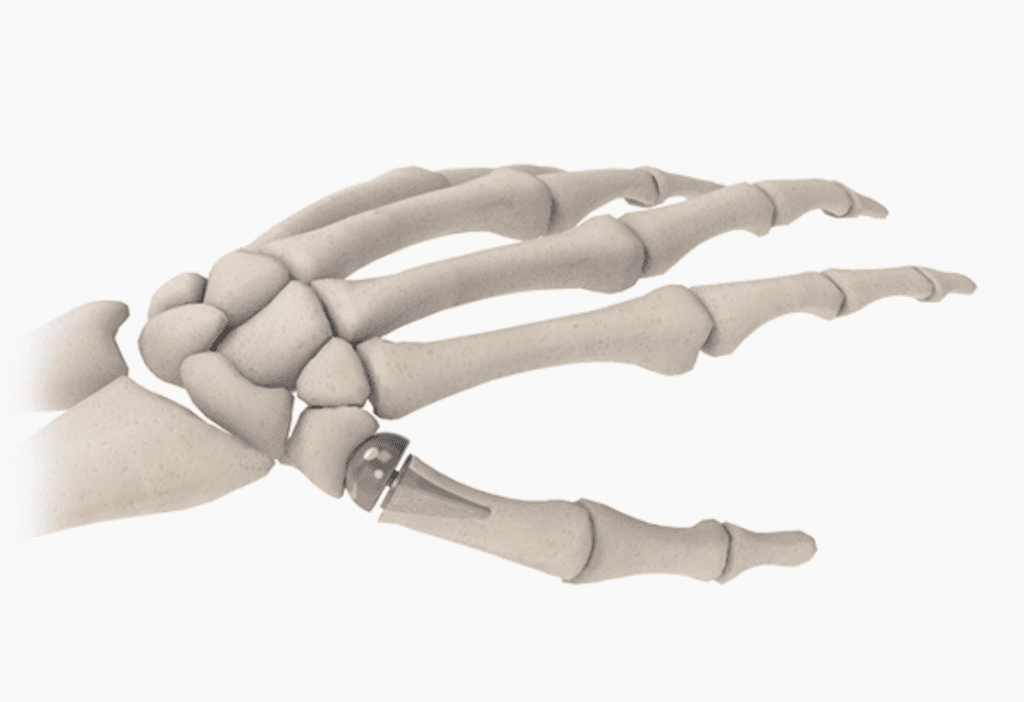
Thumb joint replacement
Like in , so many other joints, metal/polyethylene joint replacements are available and offer a good alternative in older patients where demands are less and functional recovery is rapid.
For higher demand patients, Artelon is a newer option. It consists of a polyurethane urea material that allows for an interposition arthroplasty serving as a cushion for he joint to provide pain relief.
If failure should occur, the implant can be excised and the remainder of the trapezium removed. Because the procedure requires only millimeters of trapezial bone excision, the underlying biomechanics of the thumb are maintained.
In certain scenarios, the implant may even be inserted arthroscopically (through a small fiberoptic camera) and provide a more minimally invasive procedure that accomplishes the same goals.
Currently I prefer this method of treatment for advanced basal joint arthritis in younger or active individuals, regardless of age.
Arthroscopy for thumb pain (Basal Joint Arthritis)
The role of arthroscopy may be most beneficial in the early stages of basal joint arthritis. The earliest presentation of this painful condition has few surgical options once conservative treatment has been exhausted.
It is apparent that a young, active woman may not agree to a complete open removal of a wrist bone even when her symptoms are persistent. The other surgical options discussed are also relatively aggressive for the young, active patient.
Therefore, failed conservative treatment of thumb basal joint arthritis in these patients remains a dilemma.
However, there is now a very good alternative in arthroscopy. The patient who remains symptomatic despite several cortisone injections and splinting may very well welcome a minimally invasive procedure.
Hence, arthroscopy allows doctors to treat much earlier stages of this condition in a less painful manner while giving us a true image of the joint involvement.
The same advantages that we have seen in the treatment of large joints, such as knee and shoulder, are present in this joint.
However, the full role of arthroscopy in the treatment of thumb arthritis remains to be seen. As people live longer and become increasingly more active, it will be crucial to provide better options for the painful arthritic thumb.
New advances in small joint. arthroscopic procedures or in biomaterials will lead to greater treatment options at this vital small joint.
Removal of a supporting bone or fusion of this mobile joint may continue to have a place in surgical treatment, butI suspect that over time these treatments will become only of historical significance.
Dr. Alejandro Badia