Article in Hand Clinics · June 2006
Abstract:
Osteoarthritis of the thumb trapeziometacarpal joint is a common clinical problem as well as a perplexing challenge, because of a myriad of treatment options. The fact that so many different surgical options exist for this condition attests to the fact that none of them has an optimal success rate. Or perhaps it may be that the majority of treatment options work to the satisfaction of the surgeon; hence the clinician continues to use his favorite technique, despite the fact that it may not be the most appropriate method for a particular stage of disease. One thing is indisputable: basal joint osteoarthritis of the thumb has many different clinical presentations, and one technique cannot be used for all of the different stages and all patients’ individual needs. When conservative treatment has been exhausted, there are a wide range of surgical options to choose from. Treatment should be tailored to the individual patient. The early stages of basal joint osteoarthritis are most commonly seen in middle-aged women. The literature discusses this in many instances, but rarely gives a solution to the management of these frequently active patients. The use of antiinflam-matories, splinting, and corticosteroid injections serve only as palliative measures, with none of them altering joint mechanics or affecting the articular surface itself in any manner.
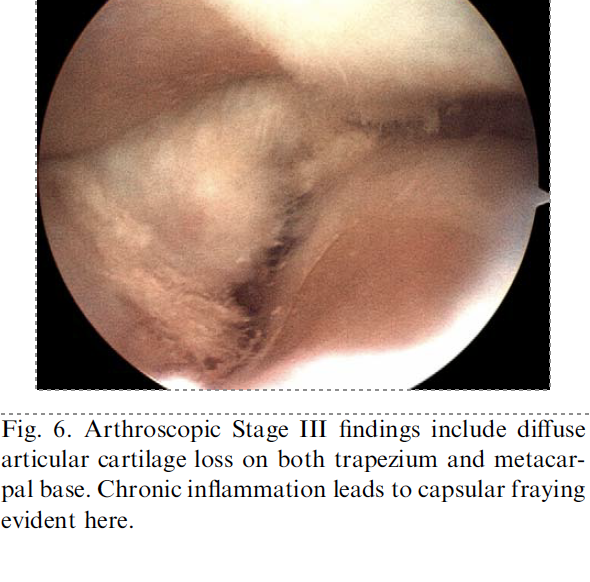
Moreover, the use of injectable steroids can accelerate cartilage loss and worsen capsular attenuation. Only the mildest cases of transient synovitis will escape the inevitable progressive loss of cartilage, and hence the need for surgical treatment if the patient indeed wants a definitive solution. After the relatively unimportant distal interphalangeal joint, the thumb carpometacarpal (CMC) joint remains the most common location for osteoarthritis in the hand. It is also the most critical for hand function. The argument has been made that man’s evolution has been largely due to the increased range of motion and function as a con-sequence of the thumb basal joint, which has led to the progressive use of tools in hominid evolution. Treatment of this functionally important joint remains a priority for the hand surgeon, and it is important to use the wide variety of surgical techniques to optimally manage this condition.
Classically, the basal joint has been treated by surgical means only when conservative options have been exhausted. The principal option has been, and remains, some type of open resectional arthroplasty. Although the literature demonstrates good results in many different studies and using a variety of techniques, it remains clear that this is a surgically aggressive procedure, because resection of an entire carpal bone is required to achieve pain relief. This certainly makes good sense in the most advanced cases in which the trapezium is typically flattened or has severe deformity includ-ing marginal osteophytes, but earlier stages demand a more conservative option that allows for future interventions if the primary treatment is not successful. Other options, perhaps less aggressive, include arthrodesis, which can provide excellent pain relief but has the obvious limitation of loss of motion, or joint replacement. Joint arthroplasty, as in any other joint in the body, has the added risk of failure of the implant, whether it be silicone or of metallic and plastic components. This is not a good option for the younger, high-demand patients.

Cite this article: Badia, Alejandro. (2006). Trapeziometacarpal Arthroscopy: A Classification and Treatment Algorithm. Hand clinics. 22. 153-63. 10.1016/j.hcl.2006.02.006.